We often look after patients with tracheostomies in cardiac ICU and usually the care of these patients is entirely uneventful.
Recently however we had an untoward event, which as a group we should reflect on.
The particular patient involved in this case was obese (this is sadly a theme in tracheostomy disasters) and had an adjustable flange tracheostomy in situ. A loss of airway occurred and respiratory arrest ensued. Luckily the patient survived.
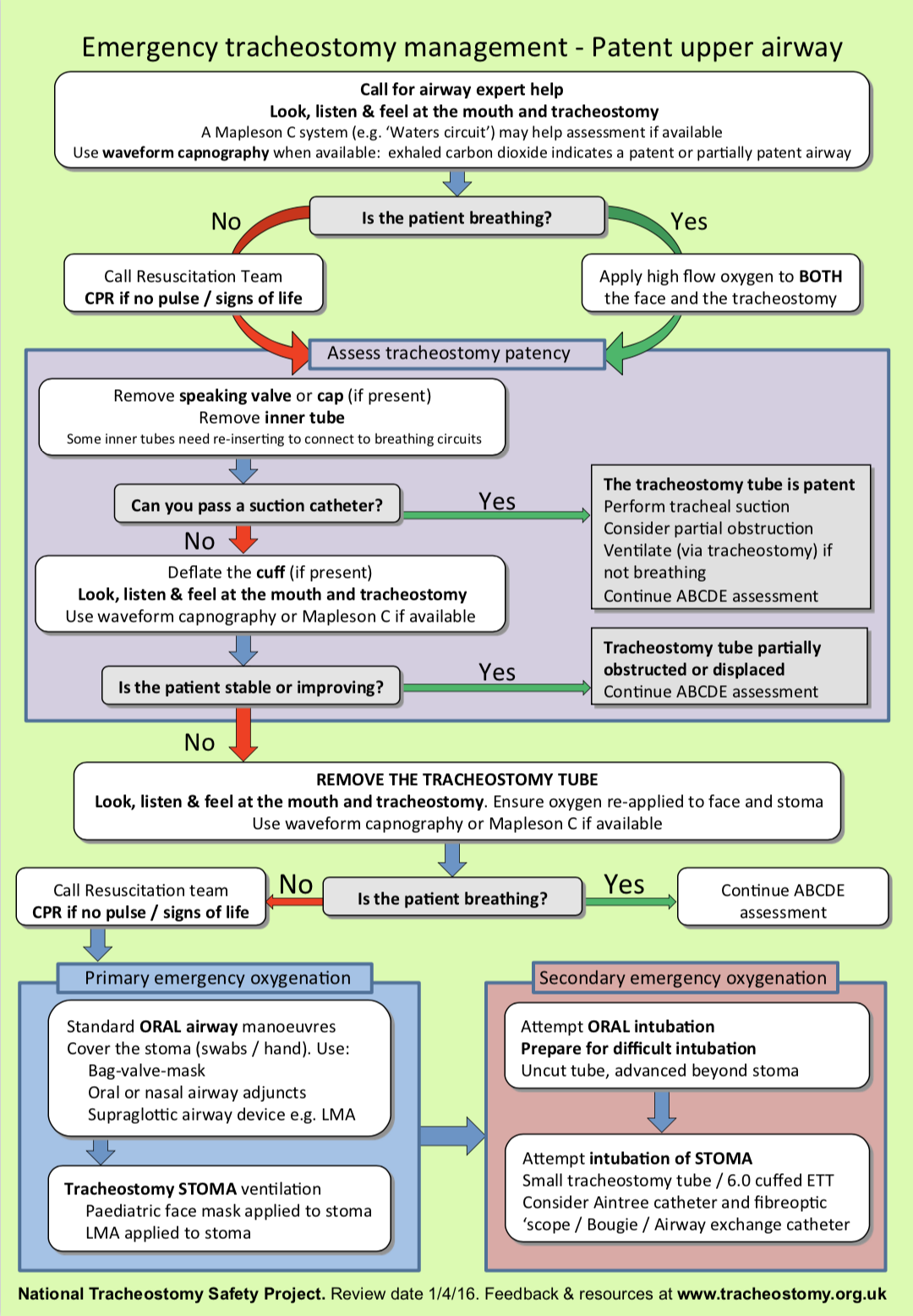
Firstly I’d like to address the emergency response management of the
displaced tracheostomy and ask that all fellows, registrars and specialty doctors working on CICU familiarise themselves with this process. An algorithm can be found here courtesy of National Tracheostomy Safety Project.
A synopsis is as follows:
– Managing this situation is stressful (I know first hand) and you will
need help to do it quickly and avoid harm
– First apply 100% O2 to the face and the tracheostomy and call for help. Do not delay this
– At UHS we use Tracoe percutaneous tracheostomy kits and these have inner tubes. They are probably the most prevalent on CICU. Portex tubes and Adjustable Flange tubes exist and not all contain inner tubes
– Inner tubes are a safety feature allowing removal of the inner part of
the tracheostomy tube which has become encrusted and blocked by secretions then safely replacing it with a patent new one
– Adjustable flange tubes are the best suited to the obese patient because they can be lengthened, allowing for the increased prettacheal soft tissue & leaving a longer segment within the trachea
– Managing the obstructed tracheostomy in CICU can best be explained by viewing the accompanied flowchart. It is a process starting with examining the inner tube (if present); is it blocked? This is evaluated by passing a suction catheter or using a fibreoptic scope if one is readily available. Do not delay things to acquire a FOB if the patient is hypoxic
– Next if still occluded, is to exclude cuff herniation as a cause of
obstruction. This is done by deflating the tracheostomy cuff. If the
patient continues to deteriorate and there is no airway the tracheostomy should be removed
– An attempt MUST be made at intubating. This can be the vocal cords or the stoma. A very large proportion of CICU tracheostomies will be easy Cormach & Lehane views at laryngoscopy. Fresh or recently sited tracheotomies close easily and are likely to be difficult to intubate.
The chance of being unfortunate enough to be in this situation is very low but if you can recall this you will have done your best for the patient. Across the trust we have blue tracheostomy boxes.
Can I also ask all trainees and fellows to look at the e-learning associated with the National Tracheostomy Safety Project. If anyone is particularly motivated or interested in further reading there is an excellent free access web site on the St George’s intranet which has a great section on tracheostomy troubleshooting. This can be found here.
Many thanks for reading and have a good week. Any feedback or discussion on this important matter will be warmly received.
Kind Regards, JM